Tailbone pain is frustrating!
- Suffering with pain day after day, week after week, month after month is incredibly frustrating.
- Life can start to revolve around the pain and how to avoid it:
- Where can I sit?
- What seats or couches do I need to avoid?
- Oh no, I forgot or lost my cushion… how am I going to make it through the day?
- What social activities can I attend?
- When is my next dose of the pain medications?
- where can I sit, what activities can I attend, when is my next dose of pain medication, etc.).
- Doctors sometimes say thoughtless things:
- Unfortunately, sometimes doctors are dismissive of patients with tailbone pain.
- Doctors may not understand what is causing your pain or how badly your suffering and how badly this condition can impair your quality of life.
- Sometimes the doctor may make an inappropriate offhand comment or joke. Perhaps he/she was trying to use humor to ease the stress of the situation, or maybe they were just being inappropriate, unprofessional, or just lacking good interpersonal skills.
- In general, when I train medical students and resident physicians here, I tell them that the safest bet is to follow the patient’s lead. Specifically, if the patient is not joking around about their pain or situation then it is definitely better if the healthcare clinicians don’t start joking around about it. This sounds simple but unfortunately many doctors say thoughtless things that harm patient care.
- If you are suffering with tailbone pain, hang in there.
- In addition to the medical treatment for the pain itself, you may want to consider seeing a professional counselor for expert guidance on how to deal with the emotional stressors that understandably occur for people suffering from chronic daily pain.
- Seek out the best medical care you can. Finding an accurate diagnosis is often a terrific source of emotional relief. Also, an accurate diagnosis lays the foundation for the optimal medical treatment plan, individualized just for you.
- Know that there is hope. Medical care constantly advances, with new treatments always on the horizon. Hang in there!
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
Tailbone pain (also called coccyx pain, or coccydynia) sometimes requires surgical treatment. Surgery to remove the coccyx is called coccygectomy.
Fortunately, the vast majority of people with tailbone pain respond well to non-surgical treatment, such as the use of cushions, medications by mouth, and coccyx injections.
For those uncommon cases where the tailbone needs to be surgically removed, patients sometimes ask whether the surgeon can give them their tailbone after it is taken out.
- In the United States, typically if a portion of the body like this is surgically removed the surgeon will send it to the pathology department where a pathologist will take a look at it just to make sure there is no evidence of cancer, etc..
- The assessment by the pathologist may be unnecessary the majority of the time, but just becomes one of those standard protocol things.
- For those who do have a surgeon willing to give them their tailbone, initially it looks pretty gross if you are not used to seeing surgical specimens and such.
- Then you would need to clean off all the muscle/tendon/etc. attachments.
- Depending on whether you had a dislocation or bony fracture you might just be left with a few separated pieces (the individual bones of the coccyx).
- Conversely, if your coccyx were entirely fused or the ligaments were still intact around the joints, you might have a solid specimen, which would make quite the conversation piece.
- Some patients have even said that they would like to hang it from a necklace!
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
How do you know if your pain is coming from something OTHER than the tailbone (coccyx)?
Or, if you do have tailbone pain (coccyx pain), how do you know if you ALSO have pain coming from other causes?
- In general, each person needs to work closely with their treating physicians to try to determine where the pain is coming from.
- This involves a combination of looking at
- how localized to the symptoms are,
- how focal the physical exam findings/tenderness are,
- how focal any imaging abnormalities are,
- how you have responded to treatments given at the tailbone versus how well you have responded to treatments at other sites
- etc.
- Consults: You may need to consult with specialists (e.g., seeing a gastroenterologist for a colonoscopy if there is concerned that the pain in the coccyx region is coming from colon cancer or anal fissure).
- Test injection: Sometimes it can be helpful if the treating pain management physician does a test injection (“diagnostic injection”) to place a small amount of local anesthetic focally at one specific spot to see if that substantially relieves the symptoms (if a tiny, focal dose of local anesthetic at one specific body location provides excellent relief of the vast majority of your pain, this helps to confirm that your pain was indeed coming from that specific part of your body).
- Some common sites of pain in the lower back and buttock region can include:
- Lumbar or lumbosacral disc herniation
- Lumbar or lumbosacral facet joint pain
- Lumbar or lumbosacral radiculopathy
- Sacroiliac joint pain
- Piriformis muscle pain
- Rectal pain
- Anal pain
- Tailbone pain
- Pelvic floor pain
- Various cancers in the pelvic and low back region
- You should work closely with your treating physicians to determine the specific location of your pain as well as the specific cause of pain at that location.
- Chapter 15 of my book (Tailbone Pain Relief Now!) talks a lot about different sources of back and buttock pain OTHER than the coccyx.
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
I am honored and excited to be part of the first ever medical conference dedicated solely to problems of the coccyx (tailbone), such as coccyx pain (tailbone pain, coccydynia).
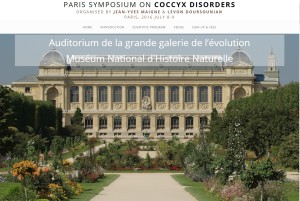
For more information, go to:
http://www.pariscoccyx2016.com/
PARIS SYMPOSIUM ON COCCYX DISORDERS
ORGANISED BY JEAN-YVES MAIGNE & LEVON DOURSOUNIAN
PARIS, 2016 JULY 8-9
PARIS SYMPOSIUM ON COCCYX DISORDERS
SCIENTIFIC PROGRAM
Auditorium de la grande galerie de l’évolution
Muséum National d’Histoire Naturelle
Friday July 8, 2016
Basic science
08:30
History of coccydynia.
by Jon Miles. Oxford, UK
08:45
Anatomy of the coccyx and related structures.
by Roger Robert. Nantes, France
09:00
Comparative anatomy.
by Cyrille Cazeau, Paris, France
09:15
Discussion
The different lesions of the coccyx and how to evidence them
09:30
Dynamic films. Technique and results.
by Jean-Yves Maigne. Paris, France
10:00
Clinical examination of the painful coccyx.
by Jean-Yves Maigne. Paris, France
10:15
MRI and CT scanner of the coccyx.
by Isabelle Pigeau. Paris, France
10:30
Discussion
10:45-11:15
Coffee break
Differential diagnosis of common coccydynia
11:15
Sacrococcygeal tumours and cysts in adults.
by Charles Court. Paris, France
11:30
Pudendal neuralgia.
by Mansour Khalfallah. Biarritz, France
12:00
Chronic anal pain and anorectal dyssynergia.
by Frédérique Le Breton. Paris, France
12:15
Neurologic and myofascial disorders mimicking coccygodynia.
by Jean-Marie Berthelot, Jean-Jacques Labat. Nantes, France
12:30
Discussion
12:45-14:15
Lunch
Conservative management of common coccydynia
14:15
Coping with coccyx pain.
by Jon Miles. Oxford, UK
14:30
Injections of the coccyx (discs and spicules). Technique and results.
by Jean-Yves Maigne. Paris, France
14:45
Ganglion impar injection.
by Patrick Foye. Newark, USA
15:00
Manual therapy for coccyx pain.
by Michael Durtnall. London, UK
15:15
Discussion
Surgical management of coccydynia
15:30
History of coccygectomy.
by Levon Doursounian & Dominique Hervault
Paris, France
15:45
Surgical technique.
by Levon Doursounian. Paris, France
16:00
Indications, follow-up and results.
by Levon Doursounian. Paris, France
16:15
Discussion
17:00
End of Day 1
17:00
Social program: a private visit of the Great Gallery of Evolution + dinner
Saturday, July 9, 2016
Free presentations
09:00
Osteotomy-fusion: a treatment for coccyx dislocation.
by Gianluca Maestretti. Fribourg, Suisse
09:15
Results of CT guided injections for coccydynia.
by Elif Gurkan. Istambul, Turkey
09:30
A Sting in the Tail.
by Michael Durtnall. London, UK
09:45
Day surgery for coccyx patients. Experiences from St. Olavs Hospital.
by Rainer G Knobloch. Tronheim, Norway
10:00
Rare lesions of the coccyx.
by Jean-Yves Maigne. Paris, France
10:15
Discussion
10:30-11:00
Coffee break
Intractable coccyx pain
11:00
Management of surgical failure.
by Jean-Yves Maigne. Paris, France
11:15
Intractable coccyx pain. What can do a pain specialist?
by Anne Lassaux. Paris, France
11:30
Discussion
Videos
11:45
Injections. Cases presentation.
by Jean-Yves Maigne. Paris, France
12:00
Closing remarks.
by Jean-Yves Maigne and Levon Doursounian
12:15
End of the Symposium
======================================
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
If an MRI shows that there is a lumbar disc herniation, could this be the cause of your tailbone pain?
Usually not.
Lumbar disc “abnormalities”
- “Abnormalities” in the lumbar discs are very very commonly seen on MRI studies.
- Sometimes these abnormal-looking discs may cause symptoms such as low back pain or nerve pain that travels down your leg.
- Perhaps even more commonly, those abnormal-looking discs might not be causing you any symptoms at all!
- It is important for the treating physician to carefully evaluate each individual patient in order to see how any such MRI findings may or may not match up with the patient’s symptoms and physical exam findings.
Lumbar vs. Tailbone
- If the patient has symptoms that are very well localized to the tailbone (coccyx), then it is very unlikely that those tailbone symptoms are coming from the lumbar spine.
- It is vastly more common that tailbone pain is actually coming from the tailbone itself.
- Let’s think about this the reverse way for a moment to see how crazy this approach is.
- In someone with lumbar symptoms (in the “small of the lower back”) it would not be automatically assumed that those lumbar symptoms are due to referred pain from the tailbone.
- Similarly, in someone with tailbone symptoms it should not be assumed that those tailbone symptoms are due to referred pain from the lumbar spine.
Problems caused by focusing only on the lumbar spine
- Unfortunately, over the years, I have seen MANY patients who saw their doctors due to tailbone pain, but the following has occurred:
- The doctor incorrectly lumps “tailbone pain” in with general “low back pain” (essentially LUMBAR pain), often without even examining the tailbone area where the patient is reporting her pain.
- The doctor orders a “LUMBAR” MRI done (which does not even include the tailbone).
- The lumbar MRI shows some “abnormal” looking findings. (In reality, the lumbar MRI findings such as a lumbar disc herniation might not be causing the patient any symptoms at all.)
- Based on the lumbar MRI “abnormalities”, the patient is subjected to various lumbar treatments, which can include:
- lumbar epidural steroid injections
- lumbar facet joint injections
- lumbar surgery
- Not surprisingly, treating the lumbar spine for problems in a totally different part of the spine (the coccyx) usually fails to give any relief at all.
- Meanwhile, the patient continues suffering while the doctor has failed to ever even examined the area of pain (the tailbone) and the doctor has failed to order the appropriate diagnostic tests for the area of pain (the tailbone).
- Because the patient has not gotten any better despite extensive treatment (at the wrong body region!), the doctor assumes that the patient’s case is hopeless or that the patient is “”crazy” or that the pain is just “all in her head”.
Take home message:
- If your symptoms are mainly localized to the tailbone area, then most likely they are being caused by a medical condition localized to the tailbone area.
- Before jumping to conclusions that the tailbone symptoms are coming from MRI “abnormalities” in the lumbar spine, be sure to see a physician who will perform a careful and thoughtful evaluation specifically at the tailbone region.
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
You may be wondering… “If I have tailbone pain, why not just have it surgically removed? Why bother trying non-surgical approaches?”
Why not just remove the tailbone right off the bat for people having tailbone pain?
- My answer would be that the vast majority of patients do well with milder and easier treatments.
- The milder treatments generally have a faster recovery time and less side effects.
- For patients who are still having pain despite oral medications, cushions, etc., then I typically use a stepwise approach regarding injections.
- For example, I often start with a local steroid injection, or sometimes a local steroid injection combined with a ganglion Impar injection (which is a type of sympathetic nerve block).
- Most patients do well with those injections, obtaining very good relief of their tailbone pain.
- For those patients who do not get enough relief, then I consider nerve ablation, which deadens or destroys the nerves that are carying the pain.
- For the limited number of patients who are still not getting enough relief, then I consider surgical consult for possible coccygectomy.
- The majority of people respond well to one of the simple more-introductory type of injections, so it makes sense to start with those simplest things first and only climb the treatment ladder as far as needed in any individual person’s case.
Regarding complications and side-effects from coccygectomy (surgical removal of the tailbone), please click on the links below:
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
- At the time of surgery to remove the coccyx (coccygectomy), it is somewhat variable what the surgeon does.
- Sometimes the tailbone is partially removed, sometimes completely removed.
- Surgeons differ in their opinions as to how important it is or isn’t to try to re-attach the pelvic floor tendons that were previously attached to the coccyx.
- After surgery, most people do not have problems due to losing the natural attachments to the coccyx.
- But perhaps 5% or less may develop a complication called pelvic floor prolapse, where the floor of the pelvis starts to sag downward, which can cause problems with bowel and bladder function.
Regarding complications and side-effects from coccygectomy (surgical removal of the tailbone), please click on the links below:
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
When there is skin breakdown of ulceration of the skin over the coccyx, it is worth looking for a cause.
- Sometimes people develop a bed-sore of the skin behind the sacrum and coccyx after spending too much time laying in bed. (The medical term for a bedsore is a “decubitus ulcer”.)
- Usually, a bedsore will heal once the person is more active (spending less time laying in bed) or with more frequent repositioning in bed (such as having the nurses or family roll the patient in bed every two hours, in order to give the skin a chance to heal and ‘breathe’).
- But in some cases the skin breakdown may persist or it may come back.
- Or sometimes the skin has delayed healing after a coccygectomy (surgical amputation of the coccyx). Normally a surgical site will close and heal, but sometimes this is delayed or there are problems with healing at the post-operative site. There may even be “dehiscence”, which is also called “wound separation.” (Dehiscence means that the edges of the wound no longer meet, and this can result in delayed healing and increased risk for the wound to become infected.)
If the skin breakdown persists or returns, consider these possible causes:
1) Infection? I would think that the first step would be trying to differentiate whether the lack of forward healing seems to be caused by an underlying infection or not. Typical signs of infection include fever, chills, redness/warmth of the skin in the area, blood work showing increased white blood cells (wbc’s), blood work showing increased ESR (erythrocyte sedimentation rate) or CRP (ESR and CRP are both general signs of inflammation, which can include infection), imaging findings of inflammation on MRI (including specifically looking to see whether any such inflammation is located within the substance of the bone [bone infection is called osteomyelitis] or whether any such inflammation is located in the soft tissue structures outside of the bone [including skin infection, which is called cellulitis]).
2) Underlying immune compromise? Particularly if there is any recurring infection, then it would be worthwhile asking your primary care doctor to check whether there is any underlying compromise of your immune system that might be putting you at risk for these persistent or recurrent infections. This would typically mean checking for things like HIV/AIDS, certain cancers especially certain leukemias (blood cancers involving the white blood cells), etc.. A consultation with an “Infectious Disease” (ID) physician specialist may be helpful.
3) Nutritional deficiencies? Admittedly, most people eating a normal diet probably do not have a nutritional deficiency that is responsible for a wound failing to heal. But it is worth considering, especially if someone is only eating some kind of very restricted diet that fails to give a balance of multiple food groups.
4) Anal fistula or rectal fistula? Sometimes people develop a small tear inside the anus or within the wall of the rectum. Eventually this can form into a tunnel or track (“fistula”). This tunnel can take stool or bacteria from the bowels into nearby tissue, causing infection of those tissues. To evaluate for this possibility typically would require seeing a gastroenterologist (a physician who is a “G.I.” [gastrointestinal] specialist). Tests for this sometimes could involve putting contrast (medical dye) into the rectum and seeing if it fills up the tunnel, which would then be visible on imaging studies done after the dye is put in place.
Treatments can vary
- Antibiotics can be given to resolve infection at the wound site.
- IV antibiotics: If the infection is located within the bone, then typically get about X. would need to be several weeks of intravenous antibiotics.
- Debridement: The physician or surgeon may need to remove some of the infected tissue. This essentially removes the bulk of the infection (bacteria).
- Coccygectomy? If there a substantial possibility that there is infection within the substance of the coccyx bones themselves (osteomyelitis = bone infection), then in addition to several weeks of intravenous antibiotics (which usually should do the job) one potential consideration would be whether to surgically remove the tailbone as a means of removing the infected bones. This would have some risks, since even without an infection being present before surgery, surgical removal of the coccyx (coccygectomy) is associated with a relatively high rate of infection during the initial weeks or months after the surgery. Presumably, cutting through infected bone would be associated with an even higher rate of infection than cases where the surgeon is cutting through bone that is NOT infected. Still, removing the infected bone would essentially be removing the bulk of the infected tissue, and even if there was some persistent infection within the soft tissue structures after the surgery, those types of soft tissue infections do tend to respond antibiotics (soft tissue infections respond much better and quicker to antibiotic treatment, as compared with bone infections).
Regarding complications and side-effects from coccygectomy (surgical removal of the tailbone), please click on the links below:
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
MRI studies of the tailbone show lots of details of the anatomy of the coccyx region.
But the doctor needs to know which images to look at for the different types of details that can be seen.
- T-1 images are best for looking at bony structures like the actual bones of the tailbone (coccyx).
- T-2 images are not as good as T-1 images at showing details of the bones.
- But T2 images are better than T1 images at detecting inflammation.
- Inflammation is important to look for, since this can be a sign of joint arthritis, joint dislocations, bone fractures, bone infections, and other abnormalities.
- “STIR” images also show inflammation (similar to T2 images).
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
After coccygectomy (surgical removal of the tailbone) as a treatment for tailbone pain (coccyx pain), should patients worry about whether sex will be painful?
- I don’t know any published research on this one way or the other, but for patients I have treated after they have had coccygectomy, I don’t recall many that have reported problems with sex after the surgery.
- It’s possible, though, that people are embarrassed to mention it or I am not asking in a way that gets the best info..
- In general, people in pain may have less interest in sex or may fear that the physical nature of sex may worsen their pain, especially pain in the pelvic area, which includes the tailbone (coccyx).
- So, anything that helps to decrease someone’s pain (whether the treatment is medications, injections, or surgery) may subsequently helped to improve their interest in sex and their ability to comfortably engage in sex.
Body position during sex: how much pressure on the tailbone?
- The specific position that the person is in during sex may also be important.
- In general, positions that put direct pressure (such as your body weight, or another person’s body weight) onto the tailbone are more likely to be painful.
- So, a person laying on their back would be more likely to have tailbone pain if they are slightly reclined, as compared with someone laying flat. (While laying flat, most of the body weight is on to the sacrum, rather than the coccyx).
- People with tailbone pain may need to work together with their partners to find the positions that are least likely to cause worsening of the tailbone pain. Examples include figuring out who should be ‘on top’.
Vaginal versus anal sex
- Also, it is important to distinguish between vaginal intercourse versus anal intercourse.
- My guess is that anal sex would potentially be much more problematic for people with tailbone pain, whether they had surgery for the coccyx or not. But again I don’t have actual research/surveys to support that, just my expectation based on the anatomy there.
To come to Dr. Foye’s Tailbone Pain Center:
Tailbone Pain Book:
To get your copy of Dr. Foye’s book, “Tailbone Pain Relief Now!” click on this link: www.TailbonePainBook.com
 Book: “Tailbone Pain Relief Now! Causes and Treatments for Your Sore or Injured Coccyx” by Patrick Foye, M.D.
|
Book Now Available! Click on the book to get it now:
|